When Retaliation Against One Doctor Becomes a Public Health Crisis
- Sharisse Stephenson
- Oct 8
- 3 min read
A Mission to Serve the Underserved
I came to Hampton Roads to serve a mission — bringing neurological care to patients who needed it most.
My clinic served Portsmouth, Virginia, a city facing some of the worst health outcomes in the country. Portsmouth ranks among the lowest nationally for breast cancer survival, and the same systemic gaps that drive that statistic exist across nearly every specialty.
This is a community that desperately needs consistent, specialized medical care — not more barriers.

A Nine-Month Waiting List for Care
Before I arrived, there was a nine-month waiting list for neurology appointments. Thousands of patients — many on Medicaid — were waiting for care, some with conditions that could lead to lifelong disability if not treated in time.
I worked through that list, reducing wait times, reopening access, and helping the health system begin advertising new neurology services for the first time in years.
But the more progress we made, the more fragile the system revealed itself to be.
A Fragile System Already Under Strain
The small group of neurologists supporting this region — one full-time physician and a handful of rotating locum providers — were stretched to their limits.
Instead of investing in them, the hospital made decisions that directly harmed every neurologist serving this community.
When the foundation is already cracking, taking away support isn’t cost-cutting — it’s collapse in slow motion.
Financial Pressure and Physician Burnout
The sole full-time neurologist before my arrival was told he owed the hospital an exorbitant sum of money and would have to take a pay cut unless he agreed to take on more hospital call coverage.
Locum providers — the safety net doctors who filled coverage gaps — were cut back because they cost more.
This left the few remaining neurologists facing impossible workloads, unfair financial strain, and unsafe patient volumes.
When Retaliation Replaces Support
Then came the retaliation — against me, the one other neurologist brought in to help.
That retaliation removed me from my role and dismantled what little safety net remained.
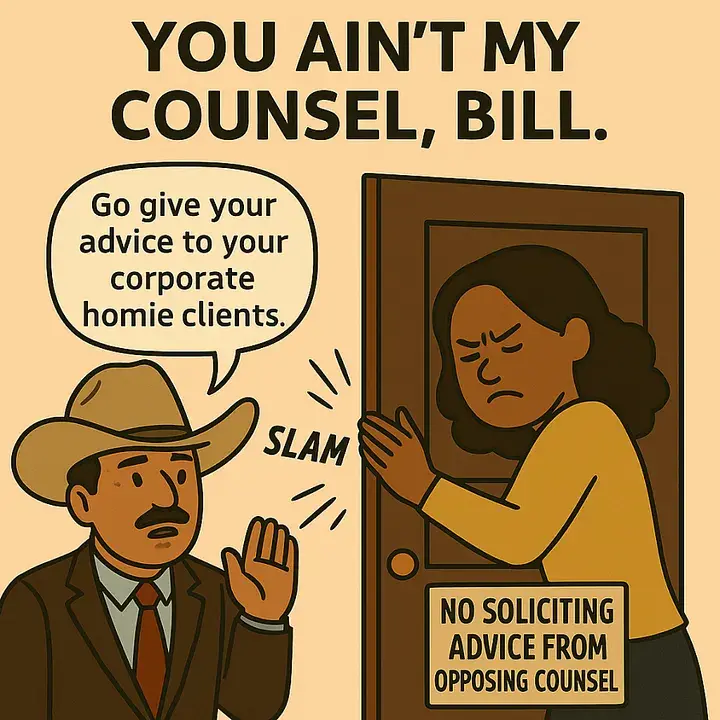
It’s unclear whether the hostility I experienced was also meant to pressure me into taking on more hospital call coverage so they wouldn’t have to pay for locums. But that was the “solution” presented to me:
“Since you’re having trouble in the clinic, why not do more call coverage? Two weeks a month for you, two for him.”
That arrangement might have saved the hospital hundreds of thousands of dollars —but it would have left clinic patients without timely care, the very thing I came here to fix.
The Collapse of a Neurology Safety Net
The end result? Every neurologist serving this community was placed under financial strain, stripped of resources, or driven out entirely.
Patients — many with Medicaid and no other access to care — are now stranded.
Those needing Botox for chronic migraine or spasticity, seizure care, stroke follow-up, and rare neurological treatment have been abandoned.
And the risk of emergency coverage gaps is higher now than it has been in years.
The Is a Public Health Crisis
When you lose neurologists in an underserved community, it’s not just an HR issue —it’s a public health crisis.
It means more ER visits.
It means longer delays for conditions that can permanently disable.
It means more people falling through the cracks in a community that can least afford it.
Portsmouth's Story Is a Warning
This isn’t just my story.
It’s Portsmouth’s story.
And it’s a warning — about what happens when the mission of serving patients is replaced by the priorities of cost-cutting and retaliation.
⚠️ Call to Action: Protect Access to Neurology Care
Patients in Portsmouth — and communities like it across the country — deserve better.
We cannot allow retaliation, intimidation, or corporate greed to dictate who gets care and who doesn’t.
Here’s how you can help:
Share this story to raise awareness about the consequences of silencing physicians who speak out.
Contact your local representatives and demand accountability for hospitals that retaliate against doctors advocating for patient safety.
Support independent and ethical healthcare providers who continue to serve underserved populations despite systemic barriers.
Follow and subscribe to the Phoenix Advocacy Network for updates, stories, and resources to take action.
When retaliation silences one doctor, entire communities lose their voice.



Comments